Your valued patients
Partnering with specialty healthcare providers to enhance the lives of patients and physicians for nearly 20 years.
1000
100
550,000
50
1000
550,000
100
50
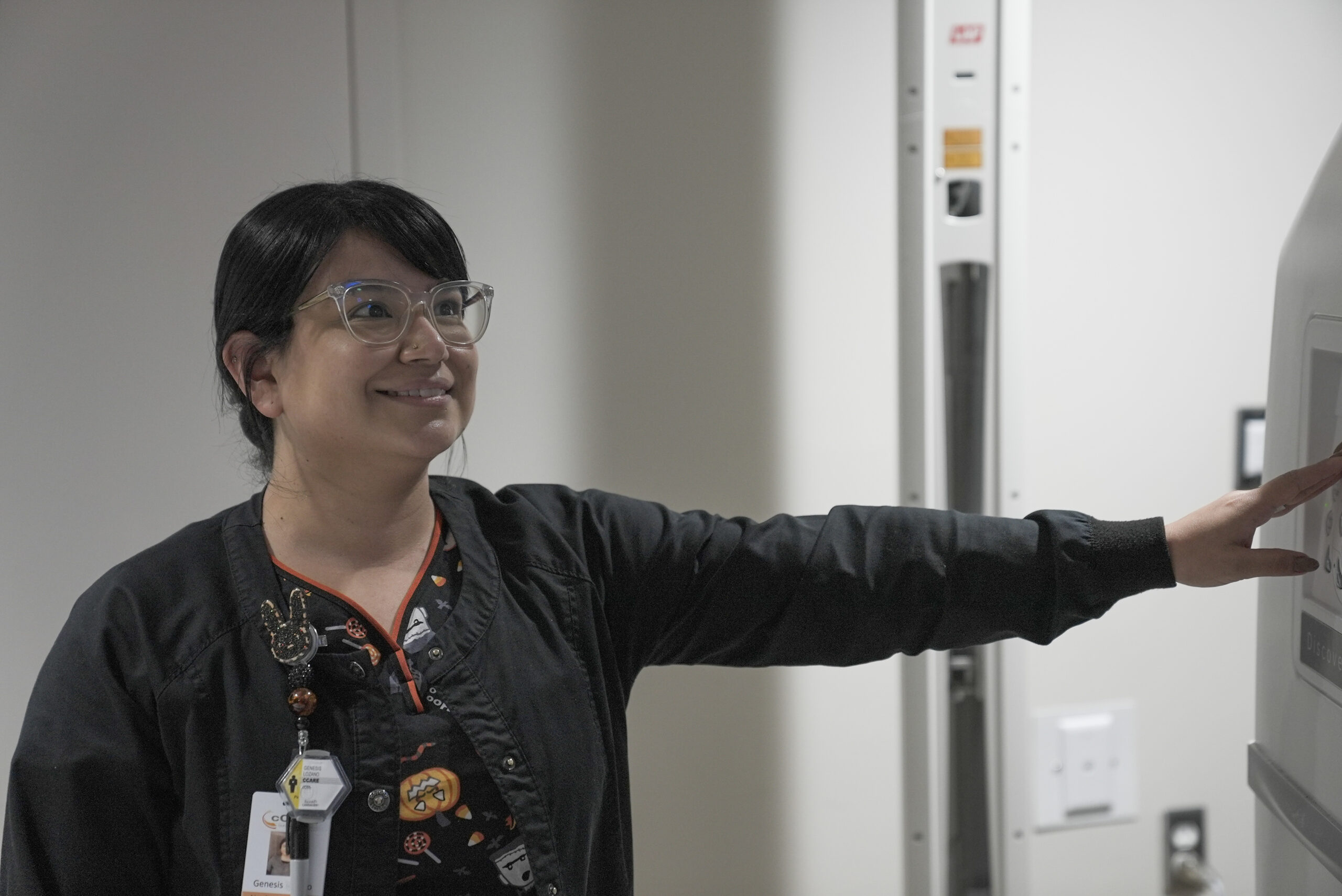
Building Value Through Community Based Programs
Empowering physicians
Our network of physicians are committed to their communities and the patients they serve. By preserving clinical autonomy, easing regulatory burdens, and providing enhancements in technology and resources, we help our physicians maintain their focus on patient care while growing a comprehensive care network for their community. Learn more about IO

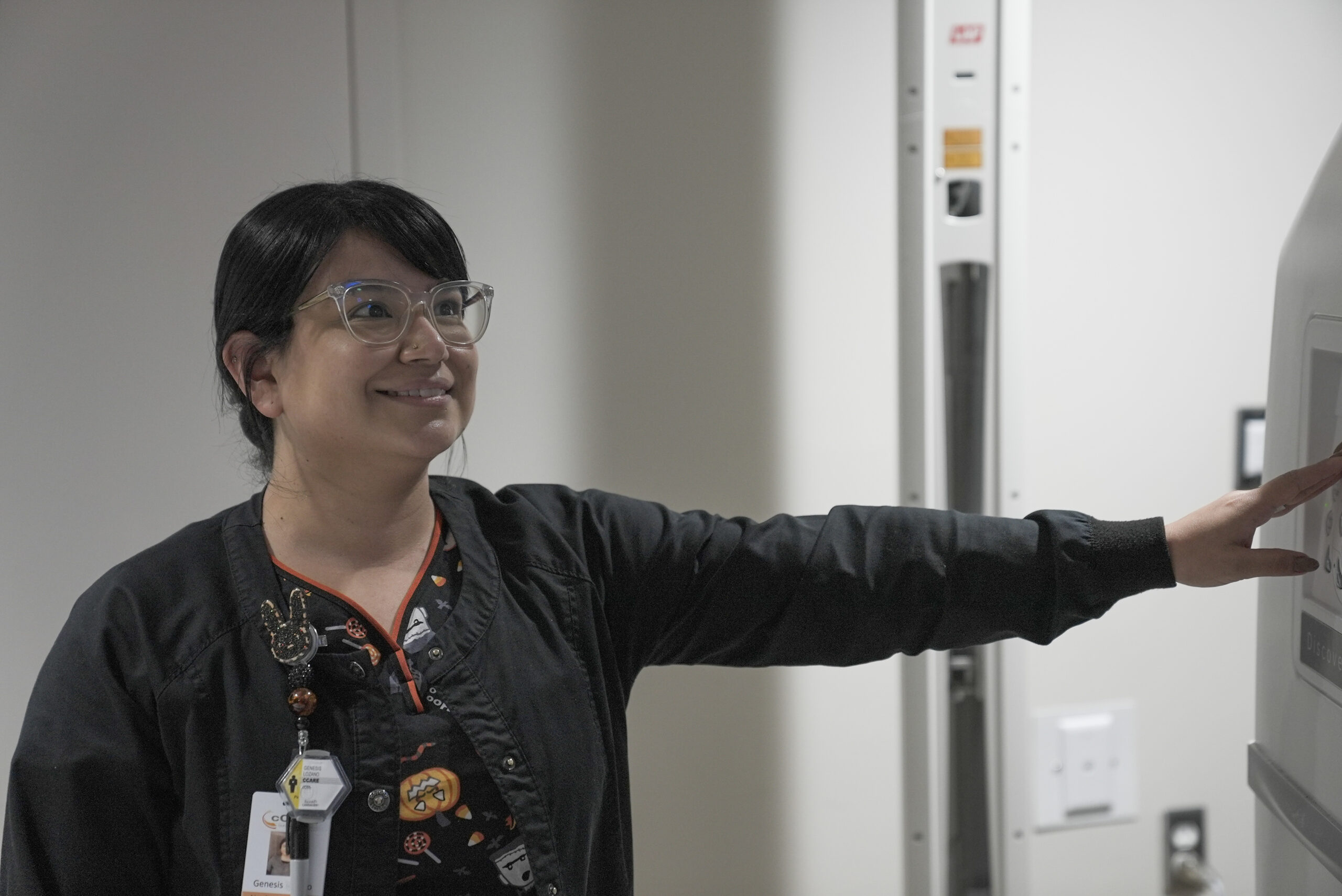
Creating Opportunity For Continued Growth
We work closely with our physicians to develop growth strategies tailored to address individual market dynamics and the unique needs of our patients. Our experienced team of operators and clinicians are dedicated to continuously evolving our community based care model to create sustained growth opportunities in each of our markets. Learn more about IO
Practice Transformation Through Innovation
In order to fully comprehend the complexity of healthcare delivery, we understand the importance of practice management across multiple platforms. Our network offers a full suite of operations support, actionable analytics, and financial management to support comprehensive care and market growth. Learn more about IO


Empowering physicians
Our network of physicians are committed to their communities and the patients they serve. By preserving clinical autonomy, easing regulatory burdens, and providing enhancements in technology and resources, we help our physicians maintain their focus on patient care while growing a comprehensive care network for their community. Learn more about IO
Creating Opportunity For Continued Growth
We work closely with our physicians to develop growth strategies tailored to address individual market dynamics and the unique needs of our patients. Our experienced team of operators and clinicians are dedicated to continuously evolving our community based care model to create sustained growth opportunities in each of our markets. Learn more about IO

Practice Transformation Through Innovation
In order to fully comprehend the complexity of healthcare delivery, we understand the importance of practice management across multiple platforms. Our network offers a full suite of operations support, actionable analytics, and financial management to support comprehensive care and market growth. Learn more about IO
Becoming a Partner
Contact Integrated Oncology Network today to start the conversation.
Becoming a Partner
Contact Integrated Oncology Network today to start the conversation.